Lesson 10: The Third Stage of Labor
"Birth is a pinnacle where women discover the courage to become mothers." ~ Anita Diamond
introduction
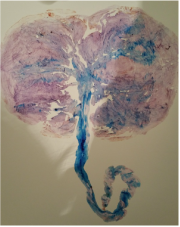 Tree of Life Placenta Print
Tree of Life Placenta Print
The third stage of labor is the most often forgotten stage. Families are so excited to meet their newborn, (and perhaps the woman is just so relieved to be done pushing!), that she sometimes forgets that the placenta still needs to be delivered in order for her to enter a non-pregnant state.
In this lesson we discuss the benefits of delayed cord clamping, as well as allowing a gentle delivery of the placenta. We also have an enlightening discussion on the reported benefits of placenta encapsulation, as well as addressing a few of the concerns surrounding the practice of placentophagia. Whatever your views on this practice, most students seem to agree on one thing for sure; this life-giving organ is amazing! After all, it supported your baby for close to ten months and deserves some respect! :)
In this lesson we discuss the benefits of delayed cord clamping, as well as allowing a gentle delivery of the placenta. We also have an enlightening discussion on the reported benefits of placenta encapsulation, as well as addressing a few of the concerns surrounding the practice of placentophagia. Whatever your views on this practice, most students seem to agree on one thing for sure; this life-giving organ is amazing! After all, it supported your baby for close to ten months and deserves some respect! :)
learning goals & focus guide
 Right Click to Download & Print This Focus Guide!
Right Click to Download & Print This Focus Guide!
After viewing and completing Lesson 10 - "The Third Stage of Labor", students will be able to:
- Name 2 possible benefits to the newborn of delayed cord clamping.
- Summarize at least 3 reasons women might choose to consume their placenta, based on anecdotal evidence.
- Identify the 2 main concerns with placentophagia expressed by Western doctors, then list how these concerns might be addressed.
- Name 2 possible benefits to the newborn of delayed cord clamping.
- Summarize at least 3 reasons women might choose to consume their placenta, based on anecdotal evidence.
- Identify the 2 main concerns with placentophagia expressed by Western doctors, then list how these concerns might be addressed.
video lesson
The Third Stage of Labor - Delayed Cord Clamping & Delivery of the Placenta
Audio Only:
resources
 A Healthy Placenta
A Healthy Placenta
~ "Prepared Childbirth: The Family Way", By Debby Amis and Jeanne Green (Your Purple Book, bottom of page 42)
~ "The Stages of Labor", by Penny Simkin
~ "Placentophagia: Benefits of Eating the Placenta: This Age-Old Tradition Has Some Surprising Benefits" by Amy Weekley
~ "The Stages of Labor", by Penny Simkin
~ "Placentophagia: Benefits of Eating the Placenta: This Age-Old Tradition Has Some Surprising Benefits" by Amy Weekley
Your browser does not support viewing this document. Click here to download the document.
diving deeper
Want to Dive Deeper? Let's Go!

~ "The benefits of delayed cord clamping still hold true when the baby is placed immediately on the mother’s chest." Vain, N.E. et al., Effect of gravity on volume of placental transfusion: a multicentre, randomised, non-inferiority trial. Lancet, 384(9939), 235-240.
~ "Something That Always Happens Right After Birth Is About To Change Forever" by Alyssa Fiorentino
~ An actively managed placental birth might be the best option for most women" ~ From MidwifeThinking.com:
"Summary: Active management of the placenta will reduced the chance of a PPH [postpartum hemorrhage] in a setting that does not support physiology and in which routine intervention is the norm. There are further options within active management that can be negotiated (see above). Physiological placental birth is an option, and possible if you manage to avoid induction, augmentation, an epidural or complications – but be aware of how difficult it may be, and don’t beat yourself up if it doesn’t happen."
~ "Something That Always Happens Right After Birth Is About To Change Forever" by Alyssa Fiorentino
~ An actively managed placental birth might be the best option for most women" ~ From MidwifeThinking.com:
"Summary: Active management of the placenta will reduced the chance of a PPH [postpartum hemorrhage] in a setting that does not support physiology and in which routine intervention is the norm. There are further options within active management that can be negotiated (see above). Physiological placental birth is an option, and possible if you manage to avoid induction, augmentation, an epidural or complications – but be aware of how difficult it may be, and don’t beat yourself up if it doesn’t happen."
Web It! Resources from The Family Way®:
reflection opportunities
|
|
Student Poll: |
Journal Entry:
Please visit the forum below under "Unit 3: Preparing For The Stages Of Labor - The Third Stage Of Labor" to reflect on the following question:
- Summarize at least 3 reasons women might choose to consume their placenta, based on anecdotal evidence.
- Summarize at least 3 reasons women might choose to consume their placenta, based on anecdotal evidence.
Please note you must log in to the forum at the beginning of each online session, even after you have already logged into the Class Portal. Click below on "Powerful Mamas Online Student Forums" to access this feature:
Inspiring Birth Stories!
"Our daughter, Charis (pronounced Care-iss), was born in a baby-friendly hospital in Austin, TX, delivered by an Ob/Gyn after 2 and a half hours of unmedicated labor and delivery. Charis' birth was a fast and furious one. Most of it is a blur in my memory.
Charis is our second child, and much like our first, I had a very challenging pregnancy. I had hyperemesis gravidarum, weekly progesterone injections starting at 18 weeks, bi-weekly ultrasounds (to monitor my cervix), pre-term labor, and 5 weeks of strict bed rest. My pre-term labor at 32 weeks left me dilated to 5 cm and 100% effaced. I listened to my doctors and did nothing other than lay down for 5 weeks, which miraculously allowed Charis to be carried to term.
The day I was released from bed rest, I headed off to the chiropractor to get my body aligned and in an optimal position for birth. I knew I couldn't waddle around for very long without labor starting. I spent most of the day with contractions on and off, but feeling really good. At 11:30 pm, my water broke and I instantly hit active labor. I knew she would come quickly because she had been engaged in my pelvis for the last five weeks. At my 37 week appointment, my doctor could actually feel her head when she checked my cervix. Basically, she was ready to come out NOW even though, based on incredibly painful back-labor, she was sunny-side up.
My husband called the hospital, our doula, and his parents to come watch our son. I waited (im)patiently, laboring in the kitchen, while my husband's parents drove to our house. As soon as they arrived, we got in the car. Thankfully we only lived five minutes from the hospital. We were admitted right away. My husband handed over our birth plan. I was quickly told that intermittent monitoring would be off the table since our daughter's heart rate was dropping significantly with each contraction. That was fine, we wanted to know she was safe in there and the monitors had long wires so I could still move. The nurses tried to let me move around a bit to get her to spin to proper position, but her heart rate continued to decelerate even more. She was wedged in there. The only position that she seemed to tolerate was me sitting on the bed slightly reclined. With contractions coming in rapid succession and all in my back, it was certainly not the most comfortable position for me. My husband and I knew she'd be arriving quickly, so we decided to not argue with the medical staff and just stay put. I could cope just fine in that position and Charis would stay safe.
Our doula had to drive all the way across the city, so she arrived when I was about 9.5 cm and just about ready to start pushing. She and the medical staff were surprised by how quickly I progressed. They called in the doctor shortly after my doula arrived. I started pushing as soon as I felt the urge to do so. The doctor ran in, sat down, and literally caught our daughter as she came flying out.
Charis' face was pretty banged up and smooshed from being wedged in my pelvis for 5 weeks and from being born sunny-side up, but she was wonderfully healthy and a petite 5 lbs. 12 oz.. The doctor put her right on my chest and she quickly found the breast on her own and began to nurse. The placenta was delivered and I had a second-degree tear that was quickly stitched up. The nurses administered her vitamin K shot while she ate and they briefly borrowed her to get her height and weight before promptly returning her to the breast. Her first feeding ended up being an hour long.
Charis' birth was incredibly fast. Even though contractions were right on top of each other and I was stuck in a bed, my husband and doula (after she arrived) were a great support team. They kept me focused when things weren't going exactly as I had hoped. I felt amazing after delivering Charis and was up, walking around as soon as she finished nursing.
Even though Charis' pregnancy was considered high risk, full of interventions, ultrasounds, medications, and bed rest, her birth was completely free of augmentations and interventions. I was so thankful that I could let my body do what it was ready to do and bring my daughter into the world quickly and naturally with a great support team at my side." ~ Lisa G.
Charis is our second child, and much like our first, I had a very challenging pregnancy. I had hyperemesis gravidarum, weekly progesterone injections starting at 18 weeks, bi-weekly ultrasounds (to monitor my cervix), pre-term labor, and 5 weeks of strict bed rest. My pre-term labor at 32 weeks left me dilated to 5 cm and 100% effaced. I listened to my doctors and did nothing other than lay down for 5 weeks, which miraculously allowed Charis to be carried to term.
The day I was released from bed rest, I headed off to the chiropractor to get my body aligned and in an optimal position for birth. I knew I couldn't waddle around for very long without labor starting. I spent most of the day with contractions on and off, but feeling really good. At 11:30 pm, my water broke and I instantly hit active labor. I knew she would come quickly because she had been engaged in my pelvis for the last five weeks. At my 37 week appointment, my doctor could actually feel her head when she checked my cervix. Basically, she was ready to come out NOW even though, based on incredibly painful back-labor, she was sunny-side up.
My husband called the hospital, our doula, and his parents to come watch our son. I waited (im)patiently, laboring in the kitchen, while my husband's parents drove to our house. As soon as they arrived, we got in the car. Thankfully we only lived five minutes from the hospital. We were admitted right away. My husband handed over our birth plan. I was quickly told that intermittent monitoring would be off the table since our daughter's heart rate was dropping significantly with each contraction. That was fine, we wanted to know she was safe in there and the monitors had long wires so I could still move. The nurses tried to let me move around a bit to get her to spin to proper position, but her heart rate continued to decelerate even more. She was wedged in there. The only position that she seemed to tolerate was me sitting on the bed slightly reclined. With contractions coming in rapid succession and all in my back, it was certainly not the most comfortable position for me. My husband and I knew she'd be arriving quickly, so we decided to not argue with the medical staff and just stay put. I could cope just fine in that position and Charis would stay safe.
Our doula had to drive all the way across the city, so she arrived when I was about 9.5 cm and just about ready to start pushing. She and the medical staff were surprised by how quickly I progressed. They called in the doctor shortly after my doula arrived. I started pushing as soon as I felt the urge to do so. The doctor ran in, sat down, and literally caught our daughter as she came flying out.
Charis' face was pretty banged up and smooshed from being wedged in my pelvis for 5 weeks and from being born sunny-side up, but she was wonderfully healthy and a petite 5 lbs. 12 oz.. The doctor put her right on my chest and she quickly found the breast on her own and began to nurse. The placenta was delivered and I had a second-degree tear that was quickly stitched up. The nurses administered her vitamin K shot while she ate and they briefly borrowed her to get her height and weight before promptly returning her to the breast. Her first feeding ended up being an hour long.
Charis' birth was incredibly fast. Even though contractions were right on top of each other and I was stuck in a bed, my husband and doula (after she arrived) were a great support team. They kept me focused when things weren't going exactly as I had hoped. I felt amazing after delivering Charis and was up, walking around as soon as she finished nursing.
Even though Charis' pregnancy was considered high risk, full of interventions, ultrasounds, medications, and bed rest, her birth was completely free of augmentations and interventions. I was so thankful that I could let my body do what it was ready to do and bring my daughter into the world quickly and naturally with a great support team at my side." ~ Lisa G.